In recent years, there has been a growing body of research shedding light on the intricate relationship between our gut and our brain. This connection is often referred to as the ‘gut-brain axis,’ and it has profound implications for our overall health and wellbeing. While the link between gut health and physical health has been recognised for some time, it’s becoming increasingly evident that our gut health also plays a pivotal role in our mental health. In this blog, we will explore the top three points that highlight the fascinating connection between gut health and mental health.
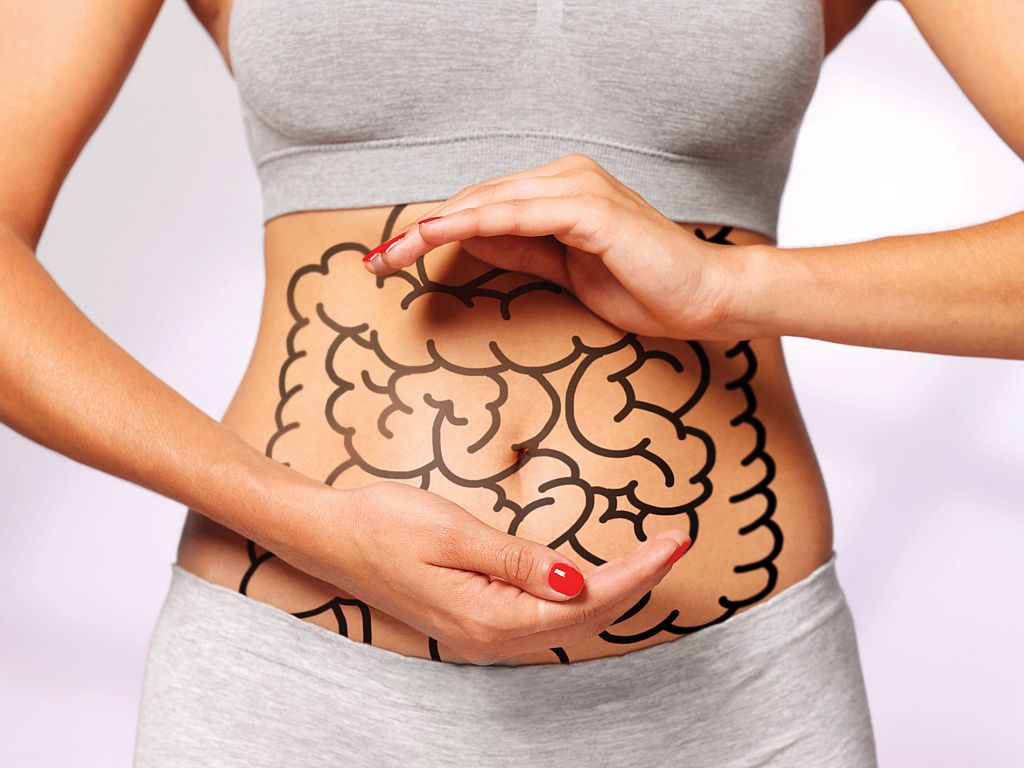
The Gut as a ‘Second Brain’
You might be surprised to learn that the human gut has sometimes been referred to as our “second brain.” This analogy isn’t just metaphorical; it’s rooted in the physiological and neurological reality. The gut contains an intricate network of neurons known as the enteric nervous system, which communicates with the brain via the vagus nerve. This bi-directional communication system allows the gut to influence the brain and vice versa.
One of the key elements of this communication is the role of neurotransmitters, including serotonin, dopamine, and GABA, which are not only produced in the brain but also in the gut. Serotonin, in particular, is of great interest in mental health as it’s a neurotransmitter associated with mood regulation. Approximately 90% of the body’s serotonin is produced in the gut. An imbalance in gut bacteria can disrupt this delicate system, potentially leading to mood disorders such as depression and anxiety.
Gut Microbiota and Mental Health
The gut is home to a vast community of microorganisms collectively known as the gut microbiota. Research in recent years has revealed that the composition of these microorganisms can have a significant impact on our mental health. The balance of ‘good’ and ‘bad’ bacteria in the gut plays a vital role in maintaining overall health and wellbeing, including mental health.
Studies have shown that an imbalance in gut microbiota, known as dysbiosis, can lead to inflammation and increased permeability of the intestinal barrier. This, in turn, can allow harmful substances to enter the bloodstream, triggering an immune response that may affect the brain. Inflammation in the body has been linked to various mental health conditions, including depression and anxiety.
Furthermore, certain beneficial gut bacteria are known to produce metabolites that can influence brain function. For instance, some gut bacteria produce short-chain fatty acids (SCFAs) like butyrate, which have been associated with reduced symptoms of depression and anxiety. These findings emphasise the importance of maintaining a diverse and healthy gut microbiota to support good mental health.
Nutritional Impact on Gut and Mental Health
What we eat has a direct impact on our gut health, which, in turn, affects our mental wellbeing. A diet rich in fibre, prebiotics, and probiotics can promote the growth of beneficial gut bacteria and help maintain a healthy gut microbiome. Conversely, a diet high in processed foods, sugar, and unhealthy fats can disrupt the balance of gut bacteria, potentially leading to inflammation and mental health issues.
In recent years, there has been a growing interest in the potential therapeutic use of dietary interventions in treating mental health disorders. The Mediterranean diet, for example, which is rich in fruits, vegetables, and omega-3 fatty acids, has been associated with a reduced risk of depression. Similarly, probiotics and fermented foods have shown promise in alleviating symptoms of anxiety and depression by promoting a healthier gut microbiota.
To support both physical and mental health, it is essential to maintain a balanced gut microbiota through a healthy diet, regular exercise, and stress management. By prioritising our gut health, we may be better equipped to maintain good mental health and enhance our quality of life.